Body composition analysis (BCA) has emerged as a critical tool in clinical medicine, offering insights into an individual’s health status, nutritional needs, and risk factors and management strategies for various medical conditions. This white paper examines the validity of current body composition measurement techniques, including most commonly utilized dual-energy X-ray absorptiometry (DXA), bioelectrical impedance analysis (BIA), and magnetic resonance imaging (MRI). It highlights the strengths and limitations of these modalities, discusses their clinical applications, and evaluates the emerging preference for MRI in comprehensive body composition analysis. It also explores the importance of measuring body composition, its relevance in patient management, clinical trials, sports performance and its role in promoting longevity highlighting studies addressing diverse populations, including minority groups and children. Evidence supports the use of body composition analysis in managing obesity, sarcopenia, and chronic diseases, while challenges remain in ensuring accurate and equitable assessment across populations.
BCA is used to describe the percentage or proportion of fat, bone and muscle in human bodies and is quickly becoming a vital indicator of health. In clinical settings, BCA is increasingly recognized as a tool for understanding overall health and managing chronic conditions, guiding nutritional interventions, and improving long-term patient outcomes. Because muscular tissue is denser than fat tissue, assessing body fat is necessary to determine the overall composition of the body, particularly when making health recommendations. Accurate measurement is vital for diagnosing conditions such as obesity, sarcopenia, and osteoporosis, and for tailoring treatment strategies. Unlike traditional metrics such as body mass index (BMI), BCA offers a more nuanced understanding of metabolic health, disease risk, and treatment efficacy. Methods like DXA and BIA have been widely used, but advanced imaging technologies like MRI are gaining prominence for their precision and comprehensiveness. This paper examines the methods used to measure body composition, evaluates their validity, and discusses their clinical relevance.
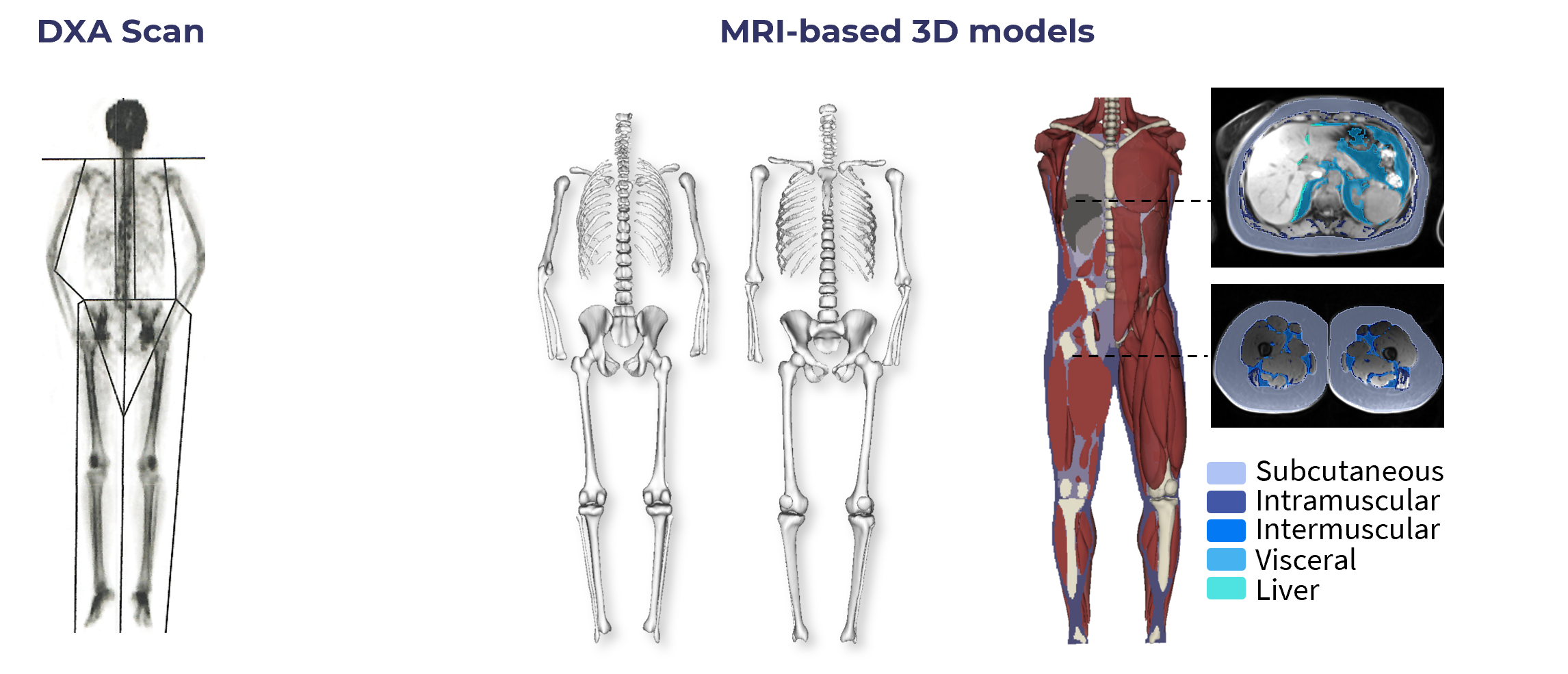
1. Dual-Energy X-Ray Absorptiometry (DXA)- DXA is a widely adopted bone mineral density assessment and provides estimates of fat mass, lean mass and regional body fat distribution. Unfortunately, DXA classifies everything that isn’t bone or fat as “lean mass,” which includes organs, water, connective tissue, and infiltrated fat. MRI studies show that infiltrated fat between and within muscles is a key driver in muscle aging and sarcopenia; these types of fat are not individually measured by DXA and, thus, DXA overestimates the amount of lean muscle present and underestimates total fat. It also does not differentiate between visceral (VAT) and subcutaneous fat (SAT). Studies indicate that DXA overestimates lean mass especially in the android regions for both men and women. DXA also appears to overestimate SAT and underestimate VAT. Furthermore, radiation exposure, although minimal, limits its use for frequent assessments. In addition, most studies indicate that it is less accurate in certain populations, including individuals with higher BMIs. DXA while excellent for population studies cannot individually measure specific adipose tissue depots.
2. Bioelectrical Impedance Analysis (BIA)- BIA is quick, portable, non-invasive and inexpensive. It estimates body composition based on electrical conductivity. Results are influenced by hydration status, recent food intake, and body temperature. It has limited accuracy in extreme obesity, children, elderly, and diverse ethnic groups.
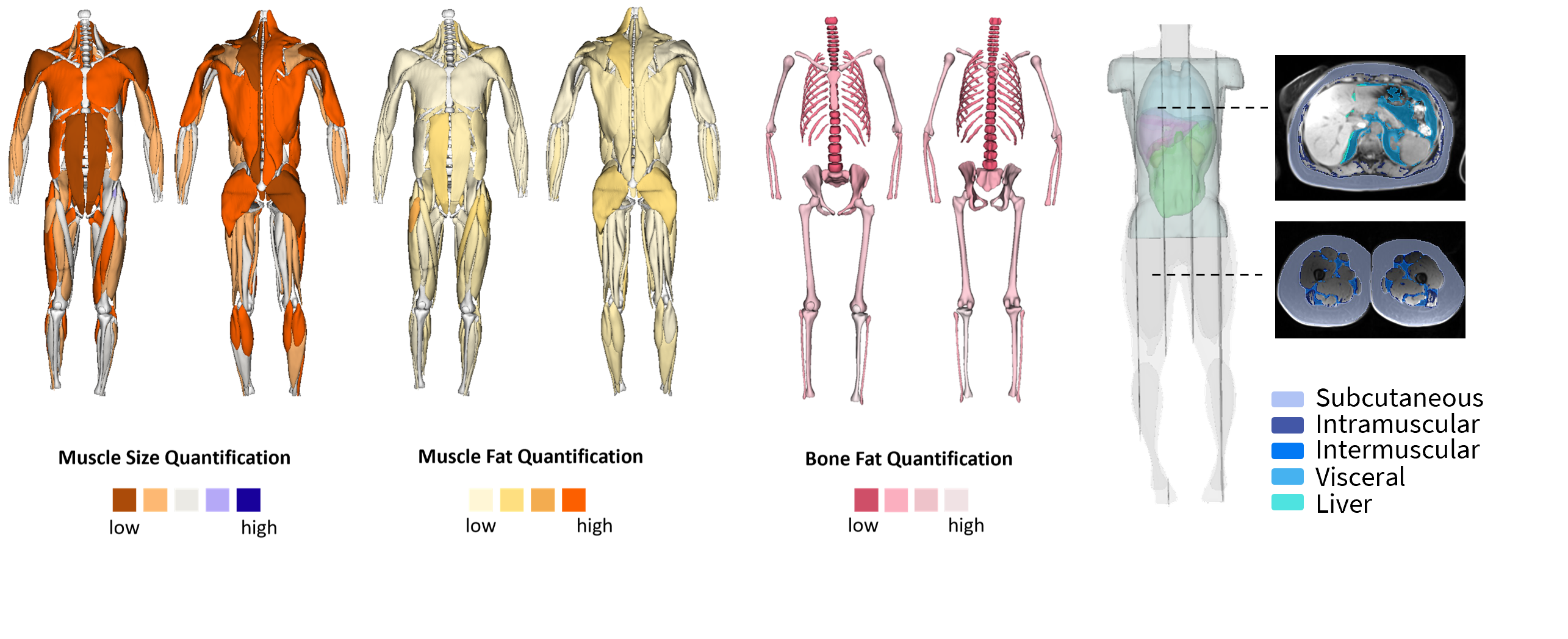
3. Magnetic Resonance Imaging (MRI)- MRI offers high-resolution imaging, allowing precise differentiation between tissue types, including visceral and subcutaneous fat, muscle quality and organs. It provides detailed body composition profiles without radiation exposure. Unfortunately, high cost and limited availability may restrict its routine clinical use and can require specialized equipment and expertise.
4. Skinfold Thickness Measurements- Inexpensive and widely accessible and useful for tracking changes over time in specific populations. However, this modality is operator-dependent, subject to significant variability and accuracy is limited compared to advanced imaging methods mentioned above.
5. Air Displacement Plethysmography (ADP)- Non-invasive and reliable for assessing fat and lean mass and suitable for diverse populations, including children, the elderly and people with disabilities. Unfortunately, it doesn't identify where fat is located on the body, results are affected by hydration status and can be expensive.
Elite Sports Performance- In elite athletics, body composition assessment is pivotal not only for optimizing performance but also for safeguarding health. Understanding muscular development, symmetry, and fat distribution supports sport-specific training, injury prevention, and return-to-play decision-making. MRI, DXA, and ADP are among the modalities used to monitor these metrics. MRI, in particular, has emerged as the gold standard for tracking changes in muscle quality and intermuscular/intramuscular fat, offering high-resolution, tissue-specific insights without exposure to ionizing radiation. This makes it especially well-suited for repeated assessments in elite populations, where precision and safety are essential. Nuanced understanding of body composition can inform training regimens, recovery strategies, and periodization to achieve sport-specific goals. As performance environments increasingly rely on objective data to guide athlete management, advanced imaging is playing a greater role in tailoring interventions and identifying risk factors that may not be apparent through functional testing alone.
Clinical Trials and Disease Management- In both clinical research and practice, body composition analysis serves as a sensitive biomarker for tracking disease progression and therapeutic response. Its role is well-established in trials involving metabolic syndrome, cancer, sarcopenia, and cachexia(where changes in muscle and fat tissue often precede shifts in traditional functional or laboratory measures). For cancer patients, particularly those with sarcopenic obesity, MRI-based assessments allow clinicians to detect muscle wasting that may be masked by high body weight. These insights prove essential to tailoring accurate chemotherapy dosing, estimating prognosis and assessing risk for treatment-related complications. Similarly, in age-related conditions like sarcopenia and osteoporosis, DXA and BIA help quantify declines in lean mass and bone mineral content, guiding interventions with dietary supplementation, resistance training, or pharmacotherapy. Clinical trials targeting nutritional rehabilitation, obesity management, or frailty in aging populations benefit from accurate, repeatable measures of fat and lean mass(where small but meaningful shifts in body composition may indicate treatment efficacy well before changes in weight or physical performance are observed).
Nutritional Assessment and Intervention- As nutrition becomes a central component of personalized care, consistent and accurate measurement tools are critical for assessing how interventions affect the structure and function of the body. Body composition analysis supports the management of both malnutrition and obesity by providing objective, quantifiable data on fat and lean mass. These insights allow clinicians to deliver more targeted nutritional interventions and evaluate their effectiveness over time. Tracking changes in body composition is especially valuable in programs focused on weight management, physical rehabilitation, or recovery from illness. In these contexts, overall weight may not reflect meaningful shifts in muscle mass or reductions in metabolically harmful fat. Imaging modalities such as DXA, BIA, and MRI can help guide and adjust dietary strategies, particularly in cases involving muscle loss, metabolic dysfunction, or inconsistent hydration status.
Disease Diagnosis and Management-
Sarcopenia: Loss of muscle mass and strength is prevalent in aging populations and is strongly associated with increased morbidity, decreased mobility, and reduced lifespan. Body composition analysis identifies at-risk individuals, allowing for targeted interventions aimed at preserving muscle health.
Obesity and Metabolic Syndrome: Studies show that visceral fat, rather than BMI or subcutaneous fat alone, correlates more closely with cardiometabolic risks. Individuals often focus on subcutaneous fat, however, visceral fat has the most significant impact on health and disease. Body composition tools can differentiate between fat compartments, offering greater insight into metabolic health. This distinction is especially important for guiding risk stratification and personalized treatment strategies in patients with normal weight but high visceral fat, or those with sarcopenic obesity.
Pediatric Applications- Body composition analysis plays a valuable role in pediatric health by supporting the assessment of growth patterns, nutritional status, and metabolic risk. It can aid in the early diagnosis of malnutrition, identify children at risk for obesity, and provide insight into the development of related conditions such as insulin resistance or type 2 diabetes. Compared to standard growth charts or BMI percentiles, body composition metrics offer a more detailed view of fat and lean mass distribution, which is particularly useful for guiding interventions during critical developmental periods. In both clinical and research settings, these insights help inform early lifestyle or medical interventions aimed at promoting long-term health outcomes.
Longevity- Body composition analysis plays a pivotal role in promoting longevity by identifying risk factors early and guiding interventions. Holmes and Racette (2021) emphasized that loss of lean mass, particularly skeletal muscle, contributes to increased risk of sarcopenia and frailty, both strongly associated with earlier mortality. Preserving muscle mass and quality is linked to improved resilience, reduced incidence of falls and disability, and better overall health outcomes in aging populations. As interest in proactive health strategies and lifespan extension grows, the ability to quantify and track these changes has become increasingly important in both clinical practice and research.
Addressing Health Disparities- Minority population studies indicate differing fat distribution patterns and metabolic risks, underscoring the need for tailored interventions. Ethnic differences in body composition (e.g., higher visceral fat in South Asians, denser bone mass in African Americans) highlight the importance of population-specific reference standards. These variations influence disease risk, treatment efficacy and response rate. To ensure accurate and equitable care, body composition tools must be capable of capturing these differences and supporting individualized evaluation across diverse populations.
Since the late 90s, DXA has been validated against accepted gold standards for body composition by comparison to chemical analysis, dissection, and anatomy‐based imaging methods (CT or MRI). MRI’s ability to generate high-quality images enables comprehensive evaluation of all body tissues. It provides detailed, volumetric assessments of body composition, allowing for accurate quantification of specific fat depots and muscle volumes, surpassing the capabilities of DXA. Studies demonstrate that MRI-based measurements have excellent repeatability and reproducibility, making them suitable for longitudinal studies and clinical assessments. MRI's ability to distinguish between different fat compartments and muscle tissues contributes to better risk stratification for metabolic and cardiovascular diseases.
Although cost and infrastructure remain barriers in some settings, advances in imaging protocols and the application of artificial intelligence to enhance its usability in clinical practice are improving the accessibility and efficiency of MRI for body composition assessment. At the same time, MRI technology has gained precision and enables more sensitive tracking over time – moving the technology from specialized research labs into commercial and high-throughput research settings.
Measuring body composition is vital in modern medicine providing detailed insights into health risks and physical status. Evidence shows that it enables tailored interventions for weight management, nutritional plans, and physical rehabilitation. It can be utilized in the clinical setting to track effectiveness of interventions over time and offers valuable data for research and public health initiatives. While DXA and BIA remain valuable tools in specific contexts, MRI offers unmatched accuracy, detail for body composition analysis, and a non-invasive, nonionizing 3D approach. Its adoption in clinical settings can revolutionize personalized healthcare, enabling precise diagnosis and targeted treatment strategies. As clinical use of body composition data continues to expand, further research and continued progress in imaging protocols, AI integration, and cost efficiency will be key to making MRI more widely accessible and impactful.